Peripheral Artery Disease - Poor Circulation
Introduction
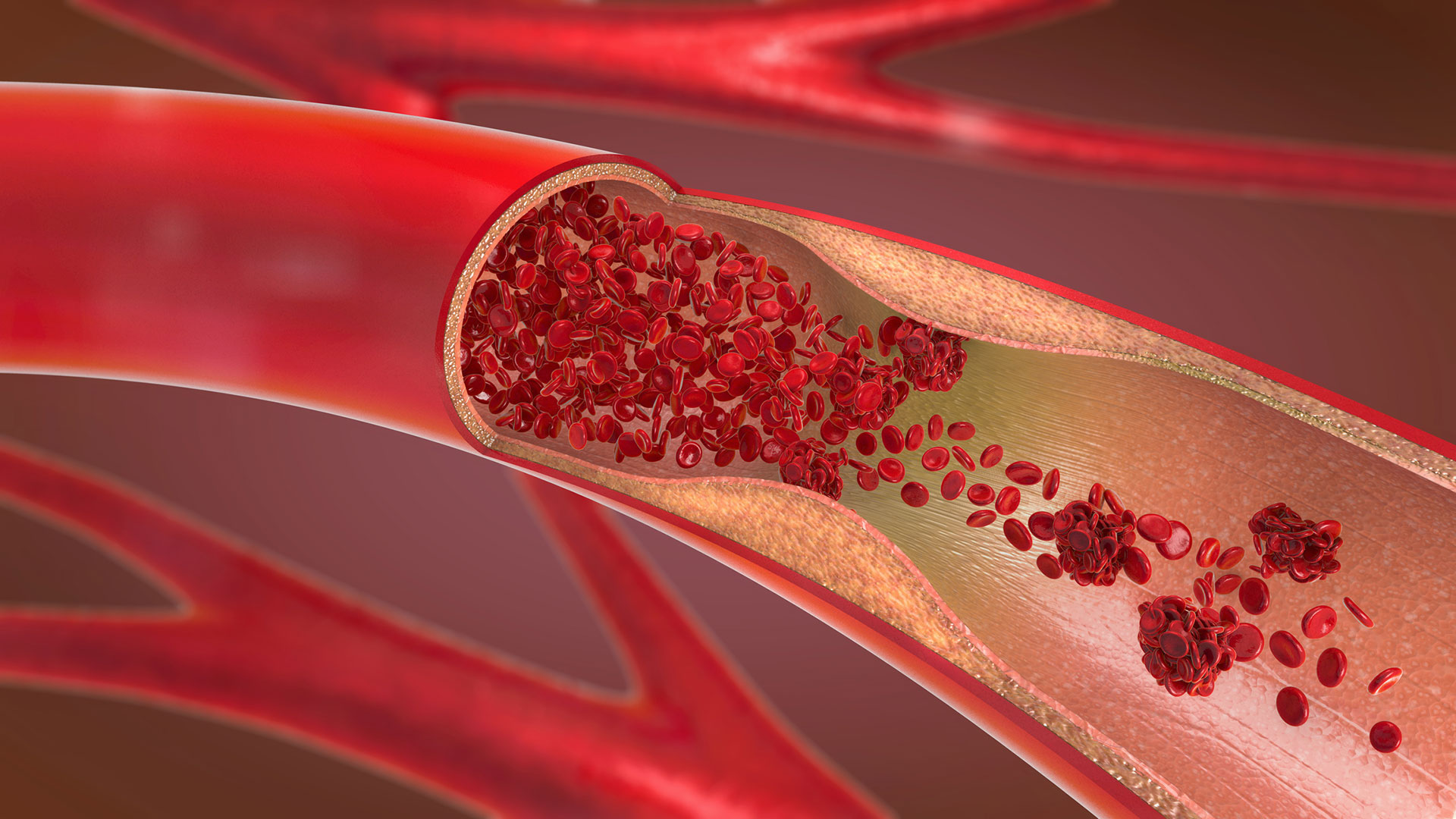
Peripheral artery disease (PAD), also referred to as arteriosclerosis of the extremities and peripheral vascular disease, is a condition that causes poor blood circulation to the kidneys, intestines, arms, legs, and feet. Blood flow may be reduced or blocked by narrowed or hardened blood vessels. This can lead to tissue and nerve injury or damage. You may decrease your risk of PAD by reducing the risk factors that you can control. PAD is treated with medications and surgery. In severe cases, amputation may be necessary.
Anatomy
The heart has several large arteries and veins connected to it that branch out and become smaller as they travel throughout your body. Your arteries and veins are blood vessels that deliver blood throughout your body in a process called circulation. Arteries carry oxygenated blood away from your heart. Veins carry deoxygenated blood from your body and lungs back to your heart.
Causes
PAD results when the arteries that supply the kidneys, intestines, arms, legs, or feet become narrow and hard. Hardening of the arteries usually develops first in the legs and feet. The arteries become less elastic, narrow, and hard because of calcium deposits on the wall of the artery. The artery may completely close, preventing blood flow. The artery may be unable to dilate (become larger) to carry more blood especially during periods of exercise. The lack of blood flow can contribute to nerve and tissue injury and damage.
Symptoms
The early symptoms of PAD usually begin in the legs and feet. It may affect one leg or both legs to different extents. The symptoms of PAD are often mistaken for something else. Leg or hip pain, cramping, and tiredness are the most common symptoms of PAD. These symptoms typically occur while walking or climbing stairs and go away with rest. You may have difficulty walking. Your legs and feet may feel numb at rest. You may experience muscle pain in your thighs, calves, and feet. Your legs and feet may feel cold and appear pale or blue. Your legs and feet may lose hair. The pulse in your affected limb may be weak or absent.
Diagnosis
A doctor can begin to diagnose PAD by reviewing your medical history, conducting a physical examination, and testing your blood. Your doctor will check the pulse and blood pressure in your limbs. Imaging tests are used to view the condition of your blood vessels.
Your doctor may perform a simple non invasive measurement in the office called ankle-brachial index (ABI) where the blood pressure is measured to determine how elastic your arteries are. A Doppler ultrasound is used to create an image of your blood vessels when a device is gently placed on your skin. Intravascular ultrasound allows a view from inside of the blood vessel walls by using a catheter device. A dye and X-ray are used to show an image of the blood vessels with an angiography. Magnetic resonance angiography (MRA) produces extremely detailed views of the blood vessels.
Treatment
PAD is treated with medications and surgery. The purpose of treatment is to relieve symptoms and improve circulation. Medications may be used to thin the blood and open the arteries to increase blood flow. Surgery may be used to repair the lining of an artery, replace the affected artery with a graft, or bypass the affected area with a synthetic blood vessel or a vein. Balloon angioplasty, stents, and laser treatments may help as well.
Prevention
You may prevent PAD by reducing the risk factors that you have control over including your weight, blood pressure, diabetes, cholesterol, and activity level. You should quit smoking. It can be helpful to exercise regularly and eat a well-balanced diet. You should make and attend all of your doctor appointments.
Am I at Risk
Risk factors may increase your likelihood of developing PAD, although some people that develop the condition do not have any risk factors. People with all of the risk factors may never develop PAD; however, the chance of developing the condition increases with the more risk factors you have. You should tell your doctor about your risk factors and discuss your concerns.
Risk factors for PAD:
_____ Cigarette smoking is a major risk factor for PAD. People that smoke may develop PAD 10 years earlier than nonsmokers.
_____ People with a personal or family history of stroke or heart disease have a higher risk for PAD.
_____ Obesity is a risk factor for PAD.
_____ Diabetes is a high risk factor for PAD.
_____ High blood pressure is a risk factor for PAD.
_____ High cholesterol is a risk factor for PAD.
_____ People with kidney disease involving hemodialysis are at risk for PAD.
_____ PAD most frequently affects men ages 50 years old and older.
_____ People that are physically inactive have a higher risk of developing PAD.
Complications
PAD may lead to foot or leg infection, sores, or ulcers. In some cases, especially among people with diabetes, amputation may eventually be necessary. PAD can lead to impotence. PAD can cause dangerous embolisms, blood clots that travel in the bloodstream.

